
10 New York Resources Helping High-Risk Communities Prevent Heart Attacks
New York Resources in today’s evolving U.S. healthcare landscape, heart health isn’t just a personal issue; it’s a public priority. Especially in high-risk communities across New York City, where poverty, stress, food deserts, and lack of healthcare access converge, the risk of heart attacks rises sharply. These communities aren’t ignoring the issue. They’re fighting back, with support, with tools, with heart.
But the road is uneven.
Some neighbourhoods benefit from world-class hospitals nearby. Others, just a subway ride away, suffer from closed clinics, underfunded outreach, and limited access to fresh food. That disparity is not just a policy failure, it’s a matter of life and death. Thankfully, NYC has mobilised a series of targeted resources that aim to change the trajectory.
Let’s dive into 10 resources and initiatives in NYC that are actively helping vulnerable populations prevent heart attacks, one small, smart intervention at a time.
Why New York Resources Matters Right Now

The U.S. healthcare system is overwhelmed by chronic disease.
Emergency departments are filled with preventable crises. Primary care is stretched. Many Americans don’t receive consistent or preventive care, and this is especially true in NYC’s underserved zip codes.
- Heart disease remains the leading cause of death in the U.S.
- Minority and low-income communities are hit hardest.
- Language barriers, cultural stigma, and mistrust of the system make prevention even more difficult.
NYC’s public health response isn’t perfect, but it’s powerful when it works.
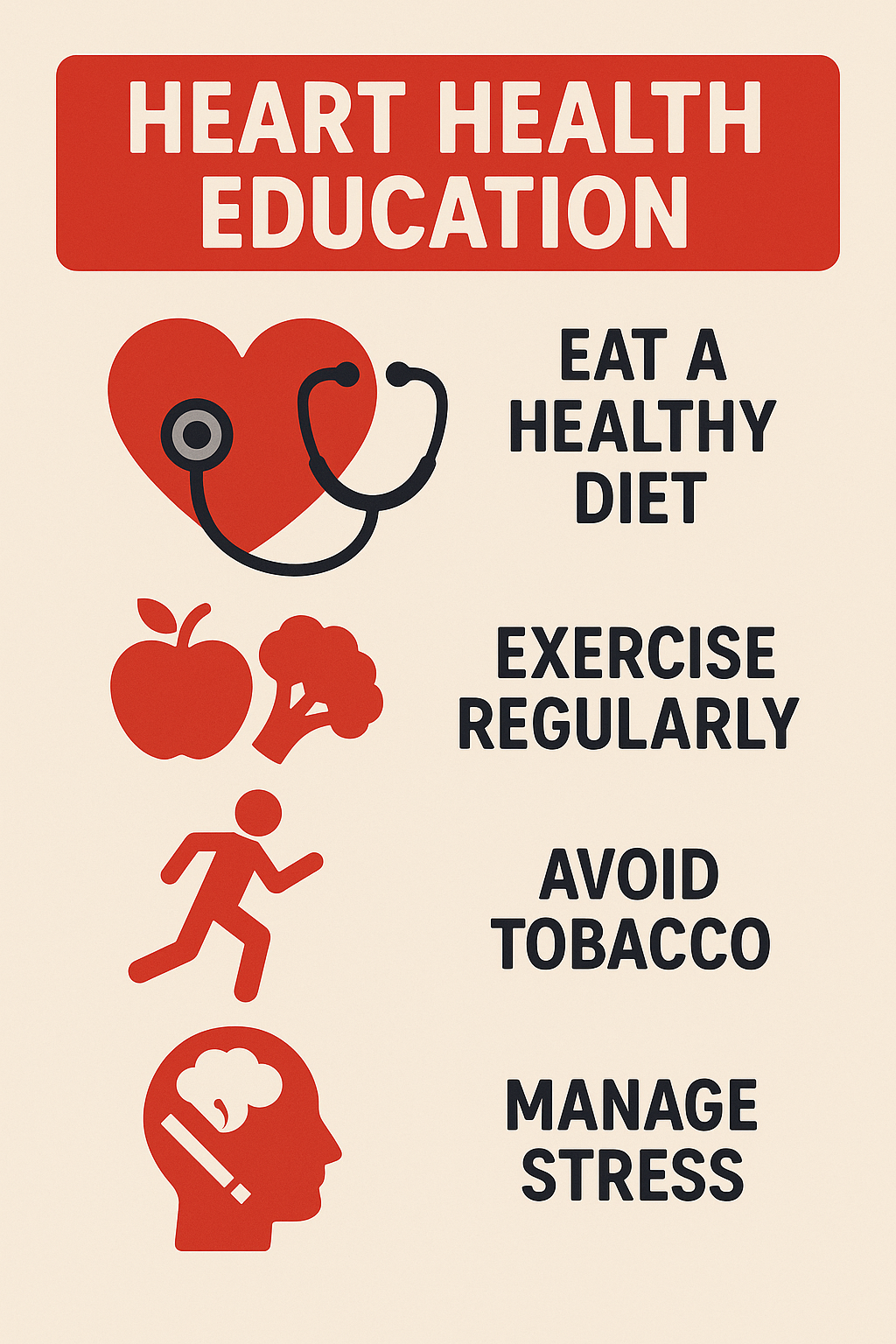
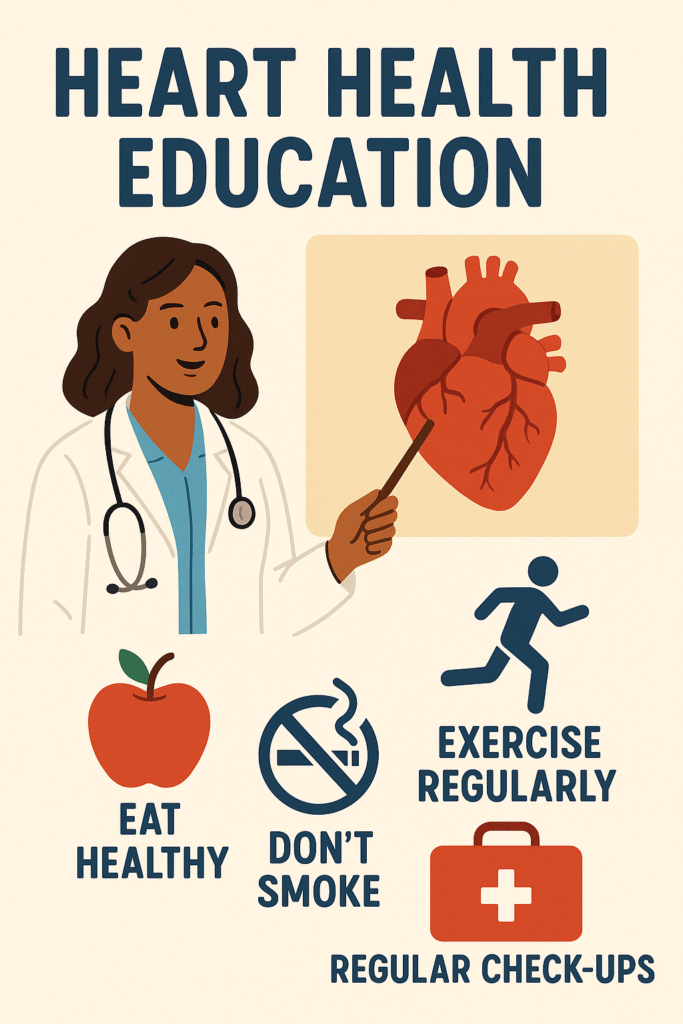
1. Community-Based Health Clinics
These clinics serve as lifelines for those without insurance or steady access to a doctor.
- Offer affordable or free screenings for blood pressure and cholesterol.
- Provide education on heart-healthy eating and physical activity.
- Connect patients with primary care and follow-up support.
Community health clinics bring prevention to the doorstep, literally.
Their presence in underserved neighbourhoods turns a once-distant health system into a neighbourhood resource. Their presence builds trust. Their presence reduces ER visits. Their presence empowers everyday decisions. Their presence saves lives.
2. Mobile Health Units
Mobile units are bridges between health deserts and real care.
- They travel to underserved areas with testing equipment.
- They offer quick blood pressure, glucose, and cholesterol checks.
- Some units also provide health coaching and referrals.
When people can’t go to the clinic, the clinic comes to them.
This mobility removes a major barrier, transportation. It also brings visibility, reminding communities that their health is not forgotten.
3. Nutrition and Wellness Programs in Low-Income Housing

Food insecurity is a silent cardiac risk.
In many NYC housing developments, programs have emerged to address this:
- Free cooking classes focused on low-salt, high-fibre meals.
- On-site nutritionists are helping residents build better habits.
- Fresh food pantries and mobile produce deliveries.
What you eat decides how your heart lives.
And when good food is placed directly in the community, not behind a paywall, it becomes a catalyst for lifelong health changes.
4. Faith-Based Health Outreach
Faith institutions remain deeply trusted, especially in immigrant and minority communities.
- Heart health workshops are hosted at mosques, churches, and temples.
- Blood pressure checks after services.
- Multilingual materials and culturally tailored advice.
Faith-based health work goes beyond science, it speaks to the soul.
When people hear about prevention in a familiar setting, they listen differently. The advice doesn’t just feel clinical, it feels personal, meaningful, and actionable.
5. Public Health Campaigns on Subway Platforms and Bus Shelters
NYC’s public health messaging gets creative, because it has to.
- Posters on the symptoms of heart attacks in women.
- Campaigns encouraging annual check-ups and cholesterol testing.
- QR codes that link to free resources or screening locations.
Every commute becomes an opportunity to spark awareness.
It may seem small, but these reminders, repeated, visible, simple, can push someone to make that overdue appointment or cut back on sodium.
6. Barbershop and Salon Health Initiatives
Yes, barbers and stylists are becoming unexpected health ambassadors.
- Barbers offer blood pressure checks during appointments.
- Salons distribute flyers on stroke and heart attack warning signs.
- Trained staff connect clients to nearby clinics.
This works because the setting is trusted. It’s familiar. It’s honest.
People sit in chairs. They share family history, stress, and fatigue. And from there, prevention becomes a conversation, not a lecture.
7. Bilingual Telehealth Services for Immigrant Populations
Language shouldn’t be a barrier to heart health. But often, it is.
- Telehealth programs now offer services in multiple languages.
- Staff are trained to address cultural taboos or misunderstandings.
- Patients can ask questions without fear of misinterpretation.
Communication isn’t just about language, it’s about clarity, trust, and comfort.
When someone hears health advice in their own words, they’re more likely to act. They’re more likely to understand. And they’re more likely to return.
8. Youth Heart Health Education in Public Schools
Prevention doesn’t wait for middle age. It starts young.
- NYC schools host fitness and health literacy classes.
- Kids learn about sodium, sugar, and stress early on.
- Parents are invited to join in workshops and cooking demos.
Education isn’t a moment. It’s a multiplier.
A child who understands their body becomes an advocate. For themselves. For their families. For the future.
9. Senior Centres Offering Cardiovascular Screenings
Older adults face higher risks, and often more isolation.
- Senior centres provide free heart screenings and walking groups.
- Workshops explain medication management and warning signs.
- Peer mentors encourage healthier choices without judgment.
Age is not a disqualifier, it’s a call to attention.
These centres don’t just provide services. They restore agency. They remind seniors that every heartbeat counts.
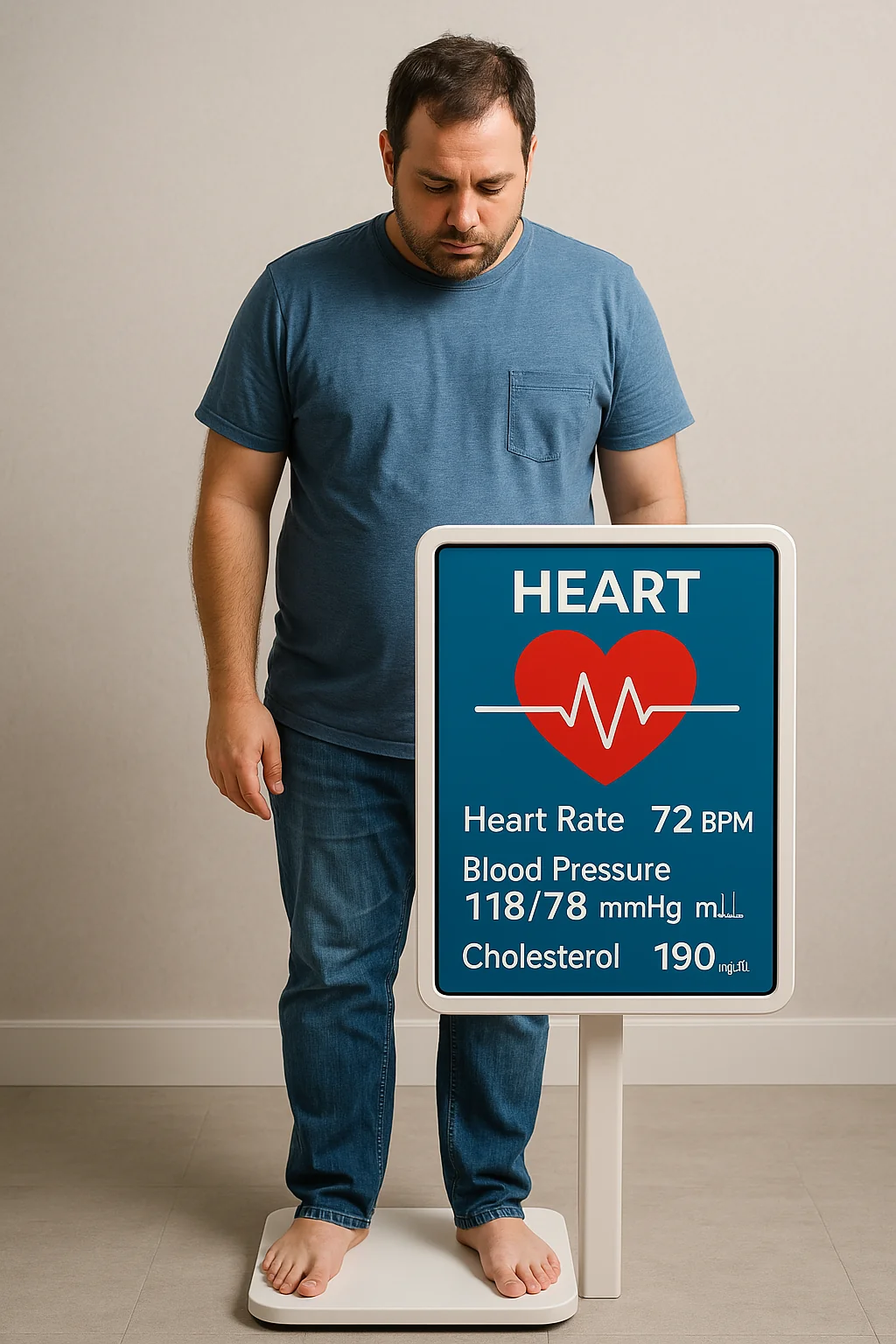
10. Heart Attack Risk Tracking Programs for People with Chronic Illness
People with diabetes, hypertension, and obesity are at much higher risk of cardiac events.
- Special programs track vitals remotely through wearable tech.
- Nurses check in weekly by phone or app.
- Personalised plans help participants manage risk factors over time.
Prevention becomes precision. Not one-size-fits-all.
Instead of waiting for symptoms, these programs aim to intercept risk early, quietly, consistently, effectively.
Stitching the New York Resources Together
These 10 resources don’t work in isolation. They’re strongest when connected.
A mobile unit refers someone to a faith-based event. A church group sends members to a telehealth app. A school invites parents to the clinic. One program feeds the next.
And that’s the only way public health truly works.
Not in silos. Not in ivory towers. But in the rhythm of the city, block by block, person by person, heart by heart.
So, Where Do We Go from Here?
We acknowledge the gaps. We recognise the flaws. We hear the frustration.
But we also see the momentum. The progress. The small wins.
And we know that every heart saved in a high-risk zip code is a sign that equity is possible.
So what now?
- If you live in NYC, explore these resources in your area.
- If you work in healthcare, build bridges between your services and these initiatives.
- If you know someone at risk, pass this along. Be the link they didn’t know they needed.
Health equity is not a wish. It’s a build. A daily build.
And today, NYC is laying brick after brick, often quietly, sometimes imperfectly, but always forward.
Because no one’s heart should fail for lack of access. Not here. Not now. Not ever.










Post Comment